Downloads
 Download
Download




This work is licensed under a Creative Commons Attribution 4.0 International License.
Editorial
SARS-CoV-2—The Autoimmune Virus Is Still Striking
Naim Mahroum 1,* and Yehuda Shoenfeld 2,3
1 International School of Medicine, Istanbul Medipol University, Kavacık, Göztepe Mah, Atatürk Cd. No:40, Beykoz, Istanbul 34810, Turkey
2 Zabludowicz Center for Autoimmune Diseases, Sheba Medical Center, Tel-Hashomer, Ramat Gan 52621, Israel
3 Reichman University, Herzliya 4610101, Israel
* Correspondence: naim.mahroum@gmail.com; Tel.: +90-216-681-5100; Fax: +90-212-531-7555
Received: 27 November 2024; Accepted: 29 November 2024; Published: 2 December 2024
Abstract: While the pandemic of COVID-19 has ended according to the WHO, new emerging cases are still documented worldwide. In addition, due to the huge number of recovered individuals, the sequelae of COVID-19 constitute a real challenge for the medical community. Of importance, is the autoimmune-nature of SARS-CoV-2. Hereby, in our editorial we aimed to shed light over the autoimmune aspects of COVID-19. Understanding the aspects presented aid in the early detection and management of affected patients.
Keywords:
infection and autoimmunity autoimmunity autoantibodies SARS-CoV-2 COVID-19We intended by our current editorial paper to summarize the features of a distinctive agent, SARS-CoV-2, and its autoimmune phenomena.
Several years ago, SARS-CoV-2, as a name, did not exist at all. However, in a short period of time, the virus reached every spot on the planet with a pandemic striking globally and aggressively. When the outbreak started, doctors (including the authors) treating patients with severe COVID-19 struggled to understand the complications seen in severely affected patients. The severe inflammatory state observed in COVID-19 patients several days after infection, was of particular implication. Among others, high C-reactive protein levels, extremely elevated ferritin values, and most importantly, the satisfactory response to systemic steroids, were significantly noticed. Based on that, and later on, COVID-19 was proposed to be considered the fifth member of the hyperferritinemic syndrome proposed earlier by Shoenfeld and colleagues [1,2]. Prior to COVID-19, the syndrome included adult-onset Still’s disease, macrophage activation syndrome, catastrophic antiphospholipid syndrome, and septic shock. With the evolution described during the pandemic of COVID-19; the role of viruses as a trigger of autoimmunity and autoimmune diseases has come back to the attention of the scientific community [3]. Historically, Epstein–Barr virus (EBV) served for decades as a strong player and presenter of autoimmune-triggering virus. Such association was consistently reported in correlation with many autoimmune diseases including, but not only, systemic lupus erythematosus (SLE) [4]. The autoimmunity-triggering abilities of these viruses, including the recently appearing SARS-CoV-2, led researchers in the field to call the viruses the “autoimmune viruses”. The term was used for the first time in regard to COVID-19, while pointing toward the association between SARS-CoV-2 and autoimmunity during the international congress of autoimmunity in 2022, approximately two years after the emergence of the pandemic [5].
The association of autoimmunity with SARS-CoV-2 infection is presented in Figure 1.
In fact, SARS-CoV-2 rightly deserved being named the autoimmune virus due to many particularities. First, while autoimmunity is fundamentally different from autoimmune disease, the earlier autoimmune manifestation of SARS-CoV-2 infection was the wide production of autoantibodies. The observed autoantibodies were of various types and directed against diverse antigenic structures. For instance, anti G-protein coupled receptors (GPCR) alongside autoantibodies against angiotensin converting enzyme (ACE) 2 have been extensively reported in association with COVID-19 [6]. The last two examples were among a list of autoantibodies including antinuclear antibody (ANA), antineutrophil cytoplasmic antibodies (ANCA), anti-interferon antibodies, lupus anticoagulants (LAC), and rheumatoid factor (RF) detected in patients with COVID-19. The clinical significance and implication of each autoantibody reported is still under active investigation. Second, SARS-CoV-2 was found to act as a trigger of autoimmune diseases. Both vasculitis and arthritis were the most described disorders to appear following the diagnosis of COVID-19 [7]. Other reported diseases, with lesser prevalence, were SLE, inflammatory myopathy, and sarcoidosis. The numerated illnesses were considered new-onset diseases due to the fact that they were diagnosed following SARS-CoV-2 infection and not before. Of importance is the hypercoagulable state seen in patients with COVID-19 necessitating treatment with anticoagulants. If added to the documented presence of antiphospholipid antibodies in people infected with SARS-CoV-2, COVID-19 was unsurprisingly addressed by us recently as another side of the coin alongside antiphospholipid syndrome (APS) [8]. Third, the immune response to SARS-CoV-2 accompanied with severe inflammatory states following infection have consistently supported the hypothesis of an autoimmune virus. Moreover, the severity of the disease was directly related to the degree of the inflammation detected. The severe inflammatory response, namely cytokine storm, was documented in COVID-19 patients with a direct correlation to mortality [9]. In addition, the levels of ferritin, as an acute phase reactant, were linked to prognosis in severe COVID-19 [1]. Fourth, after the former points being illustrated, there was no question on the critical need of systemic corticosteroids and other immunomodulators in the therapeutic arsenal against COVID-19. Such a treatment was found to increase survival in patients with pneumonia due to SARS-CoV-2 [10]. Furthermore, a meta-analysis conducted to evaluate the impact of systemic corticosteroids on the outcome of patients with COVID-19 included 71 trials with approximately 46,000 patients. The study demonstrated a decrease of all-cause mortality in COVID-19 patients treated with glucocorticoids [11].
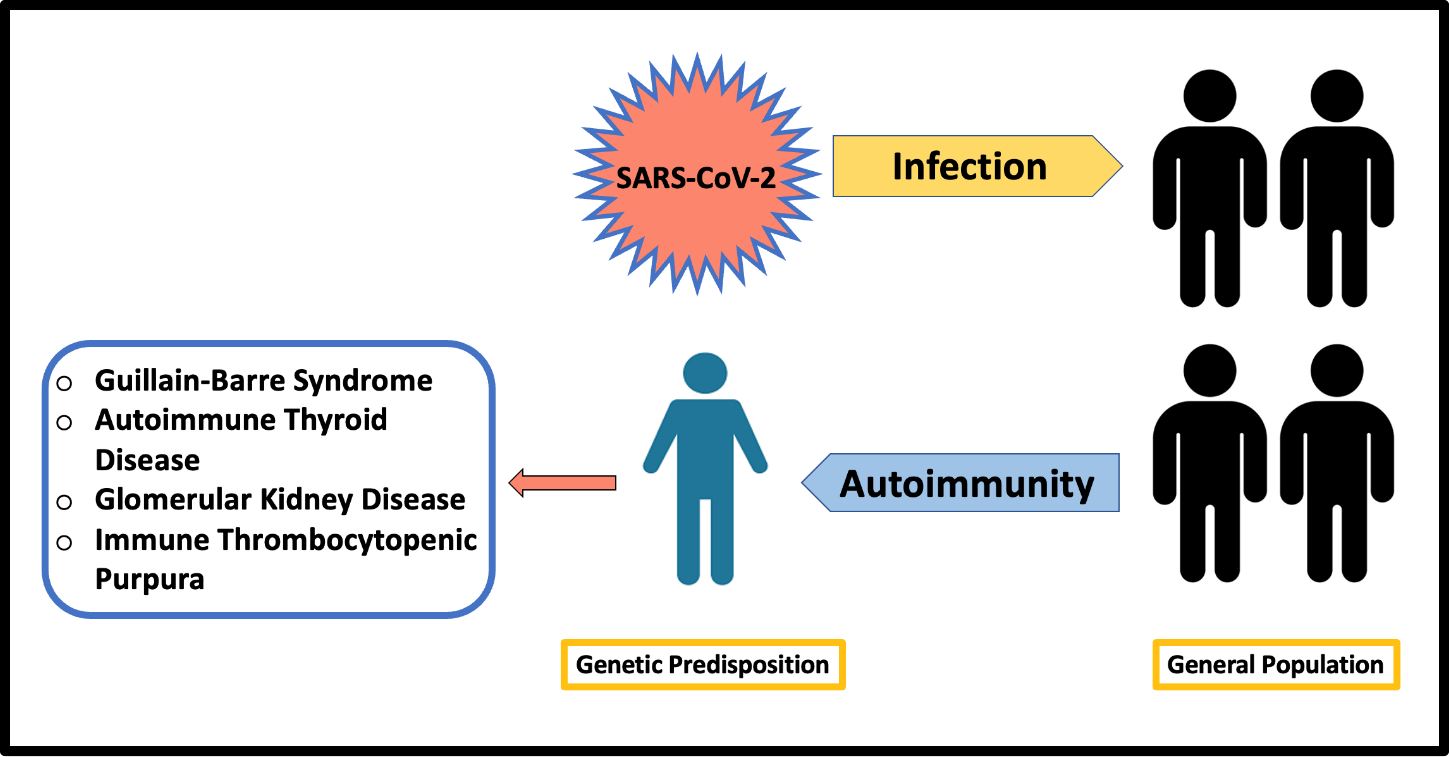
Figure 1. The association of autoimmunity with SARA-CoV-2 infection. While the number of infected persons by the virus is huge, the number of individuals who develop autoimmune manifestations are less and appear in genetically predisposed people. The autoimmune manifestations vary, and include Guillain-Barre syndrome, autoimmune thyroid disease, glomerular kidney disease, and immune thrombocytopenic purpura, among others.
While the pandemic of COVID-19 was declared ended by the World Health Organization (WHO); the sequelae of the acute SARS-CoV-2 infection is far from being so, as the autoimmune virus is still striking. The persistence of the implications of SARS-CoV-2 has manifested through three main aspects:
- New-cases: Despite the fact that the pandemic of COVID-19 was considered to have ceased; cases of SARS-CoV-2 infections are still documented worldwide. Although not in a pandemic dimension; the WHO reported more than 250,000 new cases of COVID-19 in March 2024 alone [12]. According to the same page, a surge of cases was reported during January 2024, coinciding with the winter season in the northern hemisphere. Under-vaccination or waning immunity, as well as the emergence of new strains are among the factors contributing to the recent rise. Therefore, while the link between SARS-CoV-2 and autoimmunity constitutes a challenge, the burden of SARS-CoV-2 complications, while the virus is still striking, does not seem to end soon.
- The post-COVID or long-COVID syndrome: One of the numerous features of SARS-CoV-2 is the ability of its related symptoms to persist after recovery from the acute infection. Many terms have been used interchangeably to medically describe such conditions. Post-COVID or long COVID have been used to denote the syndrome. Symptoms like cough, dyspnea, weakness, insomnia, anosmia (loss of smell), anxiety, are among the reported complaints. How is autoimmunity linked to this condition? In a follow-up of a one year period, 33 patients who recovered from acute COVID-19, were investigated for immunological and autoimmune status [13]. The enrolled patients demonstrated high levels of tumor necrosis factor-alpha, IL-17A, and IL-6, among other cytokines. Additionally, elevated levels of Th9, CD8+ effector T cells, and CD4+ effector memory T cells were detected. Altogether, the findings indicated a persistent immune activation in the post-COVID period. Similarly, post-COVID syndrome was addressed as a possible autoimmune disease in another paper [14]. The authors described a latent autoimmunity state in patients recovering from acute COVID-19 raising the possibility of an increased prevalence of autoimmune diseases in the near future.
- The COVID-19 vaccines: In addition to the acute COVID-19 association with autoimmunity; the period after infection was also correlated as mentioned earlier. Nevertheless, this was not the only link. Vaccines against COVID-19 introduced into the market in different forms and huge numbers were initially suspected to stimulate autoimmune phenomena. Later on, when data started to accumulate parallel to the increasing number of vaccinated people, more solid assumptions were made. A detailed systematic review of reported cases of COVID-19-vaccine-induced myocarditis seen in autopsy presented 28 such cases [15]. The heart was the only organ affected in the included studies. When viewed by temporal relationship, internal and external consistency among the cases, as well as the histological confirmation by autopsy, the authors concluded a high likelihood of a causal relation between COVID-19 vaccine and death due to myocarditis. Moreover, we previously described many autoimmune phenomena and diseases associated with different types of COVID-19 vaccines [16]. Hence, while vaccination against COVID-19 is still recommended up to this time, such occurrences could be reported every so often. Having said that, we do recognize the beneficial effects of COVID-19 vaccines and their role in halting the pandemic and further outbreaks. However, as we are addressing autoimmune side effects of vaccines, available data in this regard should be unveiled.
Conclusion
The autoimmune virus SARS-CoV-2 and its associated disease COVID-19 are more than an intercurrent illness that vanish following acute infection. With the severe immune response seen in acute infection, the so-called long COVID or post-COVID is only the tip of the iceberg in regard to the sequelae after infection. Of particular importance are the autoimmune phenomena ranging through a wide spectrum, from autoantibody production to autoimmune diseases requiring appropriate diagnosis and management. While the pandemic has fortunately ended, the late complications are still present and constitute a challenge for the medical community. Such conditions should be addressed, early detected, and managed appropriately.
Conflicts of Interest: The authors declare no conflict of interests.

References
- Mahroum, N.; Alghory, A.; Kiyak, Z.; Alwani, A.; Seida, R.; Alrais, M.; Shoenfeld, Y. Ferritin–from iron, through inflammation and autoimmunity, to COVID-19. J. Autoimmun. 2022, 126, 102778. https://doi.org/10.1016/j.jaut.2021.102778.
- Rosario, C.; Zandman-Goddard, G.; Meyron-Holtz, E.G.; D’Cruz, D.P.; Shoenfeld, Y. The hyperferritinemic syndrome: macrophage activation syndrome, Still’s disease, septic shock and catastrophic antiphospholipid syndrome. BMC Med. 2013, 11, 185. https://doi.org/10.1186/1741-7015-11-185.
- Mahroum, N.; Elsalti, A.; Al Shawaf, M.; Darkhabani, M.; Alwani, A.; Seida, R.; Ertas, M.T.; Simsek, A.G.; Awad, M.; Habra, M.; et al. Artificial intelligence meets the world experts; updates and novel therapies in autoimmunity–The 14th international congress on autoimmunity 2024 (AUTO14), Ljubljana. Autoimmun. Rev. 2024, 24, 103698. https://doi.org/10.1016/j.autrev.2024.103698.
- Barzilai, O.; Sherer, Y.; Ram, M.; Izhaky, D.; Anaya, J.M.; Shoenfeld, Y. Epstein-Barr virus and cytomegalovirus in autoimmune diseases: are they truly notorious? A preliminary report. Ann. N. Y. Acad. Sci. 2007, 1108, 567–577. https://doi.org/10.1196/annals.1422.059.
- Mahroum, N.; Elsalti, A.; Alwani, A.; Seida, I.; Alrais, M.; Seida, R.; Esirgun, S.N.; Abali, T.; Kiyak, Z.; Zoubi, M.; et al. The mosaic of autoimmunity–Finally discussing in person. The 13(th) international congress on autoimmunity 2022 (AUTO13) Athens. Autoimmun. Rev. 2022, 21, 103166. https://doi.org/10.1016/j.autrev.2022.103166.
- Damoiseaux, J.; Dotan, A.; Fritzler, M.J.; Bogdanos, D.P.; Meroni, P.L.; Roggenbuck, D.; Goldman, M.; Landegren, N.; Bastard, P.; Shoenfeld, Y.; et al. Autoantibodies and SARS-CoV2 infection: The spectrum from association to clinical implication: Report of the 15th Dresden Symposium on Autoantibodies. Autoimmun. Rev. 2022, 21, 103012. https://doi.org/10.1016/j.autrev.2021.103012.
- Gracia-Ramos, A.E.; Martin-Nares, E.; Hernandez-Molina, G. New Onset of Autoimmune Diseases Following COVID-19 Diagnosis. Cells 2021, 10, 3592. https://doi.org/10.3390/cells10123592.
- Mahroum, N.; Habra, M.; Alrifaai, M.A.; Shoenfeld, Y. Antiphospholipid syndrome in the era of COVID-19–Two sides of a coin. Autoimmun. Rev. 2024, 103543. https://doi.org/10.1016/j.autrev.2024.103543.
- Hu, B.; Huang, S.; Yin, L. The cytokine storm and COVID-19. J. Med. Virol. 2021, 93, 250–256. https://doi.org/10.1002/jmv.26232.
- Fernandez-Cruz, A.; Ruiz-Antoran, B.; Munoz-Gomez, A.; Sancho-Lopez, A.; Mills-Sanchez, P.; Centeno-Soto, G.A.; Blanco-Alonso, S.; Javaloyes-Garachana, L.; Galan-Gomez, A.; Valencia-Alijo, A.; et al. A Retrospective Controlled Cohort Study of the Impact of Glucocorticoid Treatment in SARS-CoV-2 Infection Mortality. Antimicrob. Agents Chemother. 2020, 64, 01168-20. https://doi.org/10.1128/AAC.01168-20.
- Li, J.; Liao, X.; Zhou, Y.; Wang, L.; Yang, H.; Zhang, W.; Zhang, Z.; Kang, Y. Comparison of Associations Between Glucocorticoids Treatment and Mortality in COVID-19 Patients and SARS Patients: A Systematic Review and Meta-Analysis. Shock 2021, 56, 215–228. https://doi.org/10.1097/SHK.0000000000001738.
- World Health Organization. WHO COVID-19 Dashboard; World Health Organization: Geneva, Switzerland, 2024.
- Acosta-Ampudia, Y.; Monsalve, D.M.; Rojas, M.; Rodriguez, Y.; Zapata, E.; Ramirez-Santana, C.; Anaya, J.M. Persistent Autoimmune Activation and Proinflammatory State in Post-Coronavirus Disease 2019 Syndrome. J. Infect. Dis. 2022, 225, 2155–2162. https://doi.org/10.1093/infdis/jiac017.
- Anaya, J.M.; Herran, M.; Beltran, S.; Rojas, M. Is post-COVID syndrome an autoimmune disease? Expert Rev. Clin. Immunol. 2022, 18, 653–666. https://doi.org/10.1080/1744666X.2022.2085561.
- Hulscher, N.; Hodkinson, R.; Makis, W.; McCullough, P.A. Autopsy findings in cases of fatal COVID-19 vaccine-induced myocarditis. ESC Heart Fail. 2024. https://doi.org/10.1002/ehf2.14680.
- Mahroum, N.; Lavine, N.; Ohayon, A.; Seida, R.; Alwani, A.; Alrais, M.; Zoubi, M.; Bragazzi, N.L. COVID-19 Vaccination and the Rate of Immune and Autoimmune Adverse Events Following Immunization: Insights From a Narrative Literature Review. Front. Immunol. 2022, 13, 872683. https://doi.org/10.3389/fimmu.2022.872683.






