Downloads
 Download
Download




This work is licensed under a Creative Commons Attribution 4.0 International License.
Review
Detoxification of Paraquat: Scooping up the Moon from the Water?
Yanyan Zhu and Xiuping Chen *
State Key Laboratory of Quality Research in Chinese Medicine, Institute of Chinese Medical Sciences, University of Macau, Macao SAR, 519000, China
* Correspondence: xpchen@um.edu.mo; Tel.: +853-88224679
Received: 9 May 2024; Revised: 6 June 2024; Accepted: 12 June 2024; Published: 23 August 2024
Abstract: Paraquat poisoning is a global public health problem, particularly in the Asia-Pacific region. Ingestion of even small amounts of paraquat can be life-threatening. However, there is no specific antidote for this pesticide, which has a low lethal dose and high lethality in humans. Paraquat poisoning causes systemic toxicity with the primary target organ being the lungs, resulting in acute alveolitis and pulmonary fibrosis. It can also lead to multiple organ failure. This review summarizes the current clinical management of patients with paraquat poisoning and the potentially effective compounds reported in the literature and patents for the treatment of paraquat poisoning. It also summarizes future directions for antidote development based on reports of available potential antidotes and provides ideas for paraquat antidote development.
Keywords:
paraquat poisoning detoxification1. Introduction
Paraquat (PQ) is a non-selective quaternary herbicide that was once widely used in agriculture because of its low price, high weed control efficiency, soil inactivation, and minimal residue in the soil [1]. However, PQ is also highly toxic to humans. According to statistics, 14–20% of all suicides worldwide are caused by pesticide ingestion, with PQ ingestion being the most deadly form of pesticide suicide [2].
PQ induces toxicity throughout the body but preferentially affects the lung and kidney [3]. However, the exact mechanisms of PQ toxicity remain unclear. It is generally accepted that PQ enters the lung and first undergoes a redox cycle to produce free radicals to damage the mitochondria in lung cells, resulting in mitochondrial damage [4]. This is followed by the release of large amounts of unwanted electrons from the mitochondria into the cytoplasm, leading to oxidative stress [5]. In addition, oxygen free radicals generated during oxidative damage led to lung fibrosis through both reactive and inactive oxygen pathways. If an overdose of PQ (20 mL, 20% concentration of the drug) is ingested, most patients will die within 3 days due to multiple organ failure [6]. As a result, PQ was quickly classified as a ‘restricted use’ herbicide due to its high lethality and the absence of a specific antidote [7]. Today, PQ is banned in most countries but is still very popular in some developing countries [8]. Its high lethality to humans and its high efficiency and low cost in weeding become its two faces. The application of PQ has greatly promoted global food production and ensured food security in the last century [9]. It is a pity to ban PQ because there is no better alternative herbicide available. The development of PQ antidotes has been going on for many years with little success. We wonder, does a PQ antidote exist? Are our efforts to explore PQ detoxification drugs a waste of money? This brief review summarizes the current research findings, analyses the treatment strategies, and discusses the potential PQ antidotes developed in recent years. In particular, we suggest several possible future directions for further research.
2. Current Management for PQ Poisoning
2.1. Gastric Lavage
Patients with PQ poisoning is generally treated differently depending on the dose and time of PQ ingestion (Figure 1). In patients with PQ poisoning, if the patient is conscious without vomiting, the ingestion dose is less than 20 mg/kg and the ingestion time is less than one hour, gastric lavage may be considered using adsorbents, the choice of which includes activated carbon and bleaching earth [10].
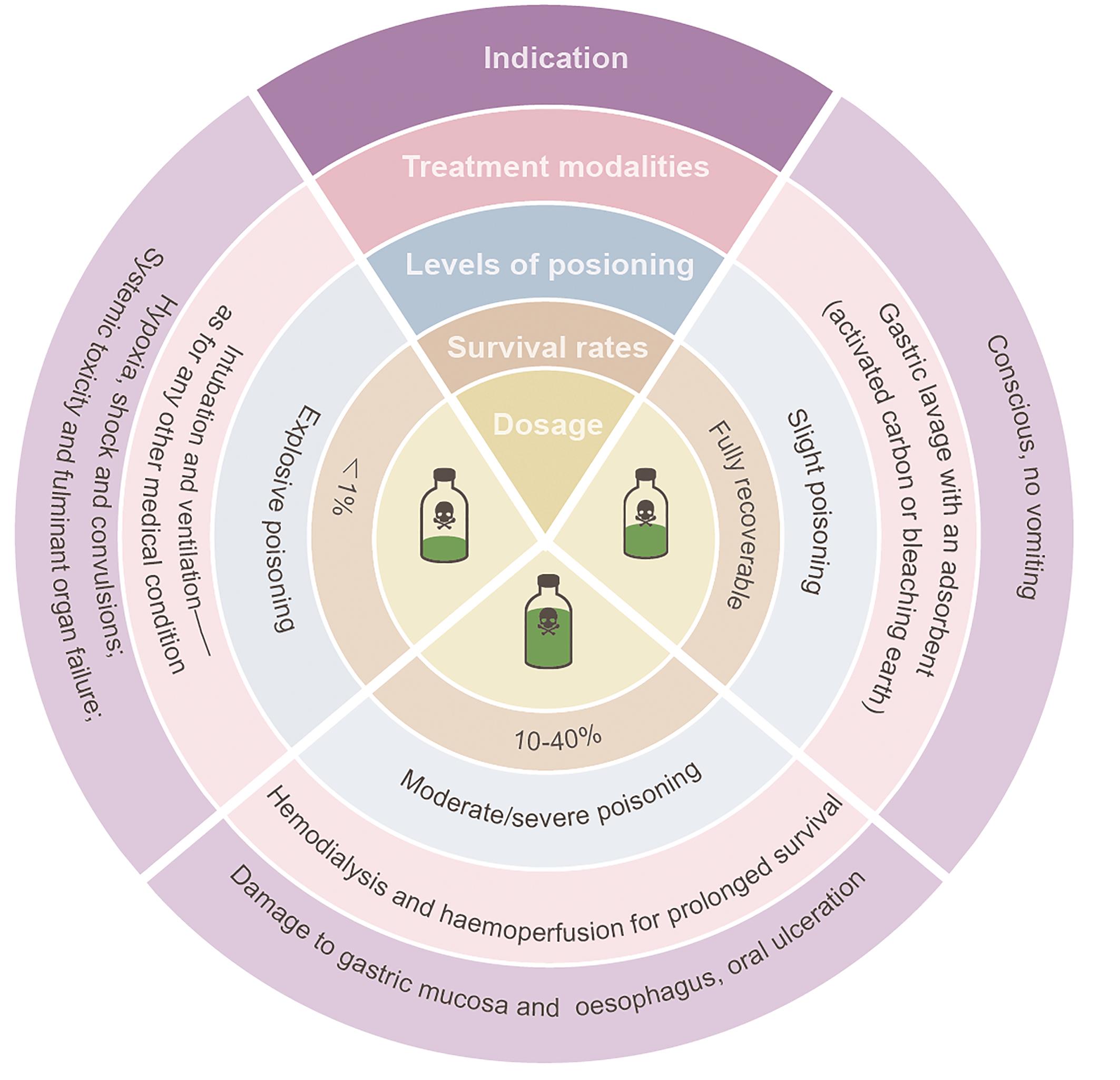
Figure 1. Grades of paraquat poisoning and treatment measures in clinical settings. 534 × 522 mm (59 × 59 DPI).
2.2. Hemodialysis
If a patient ingests 20–40 mg/kg, this is clinically considered “moderately severe poisoning”, and the patient may develop renal failure within 2–6 days of ingestion. Worse, acute pulmonary alveolitis may develop early, with pulmonary fibrosis occurring within five weeks or so, leading to death from hypoxic respiratory failure. The mortality rate for moderately severe patients is well over 50% [11,12]. The clinical management of these patients is mainly based on hemoperfusion and hemodialysis [6,13,14]. It has been reported that combined continuous intravenous hemofiltration and hemoperfusion treatment of patients who ingested PQ within 48 h significantly improved patient survival at 90 days [15]. However, hemoperfusion is not useful for patients who have ingested a lethal dose of PQ. Emergency treatment such as intubation and ventilation is often used for such patients, but unfortunately, most of them deteriorate within a few hours and will die within 1–4 days [16].
2.3. Available Drugs
Since there is no specific antidote for PQ poisoning, the physician will use one or more of the following methods to treat the patient, with the patient’s consent, depending on the patient’s condition [17]. The pharmacological treatment falls into two main directions, immunosuppression and high doses of antioxidants administration.
The combination of cyclophosphamide, a commonly used chemotherapeutic agent with immunosuppressive as well as immunomodulatory properties, and glucocorticoids may reduce the risk and mortality in patients with PQ intoxication in clinical practice [18,19]. In a case pathology report from Taiwan in 2002, a severe case of PQ severity was successfully treated clinically with repeated methylprednisolone shock therapy and high-dose dexamethasone [20]. However, the sample size of this result is too small to directly determine whether this treatment can effectively alleviate PQ toxicity.
When PQ enters the body, it triggers the release of oxygen free radicals which deplete the body of antioxidants [4]. Therefore, antioxidant administration to treat patients with PQ poisoning is a possibility. High doses of vitamin C have antioxidant activity and can scavenge oxygen radicals. Clinical case studies have shown that the survival rate of 10 patients in the high-dose combination of vitamin C and vitamin E was 50% compared with 9 deaths in the conventional treatment group, suggesting that high-dose antioxidant treatment is effective in improving the survival rate of PQ poisoned patients [21]. Another statistic showed that high doses of long-term antioxidant therapy combined with conventional treatment such as hemoperfusions significantly improved the survival rate of PQ-poisoned patients and reduced pulmonary fibrosis in poisoned patients [22]. In contrast, conventional doses of antioxidants showed no significant effect on the survival rate of patients with PQ poisoning [23,24].
3. Current Progress in PQ Detoxification Drug Discovery
3.1. Potential Leads in Patents
PQ poisoning is rapidly distributed throughout the body, causing damage to multiple target organs, primarily affecting the lungs, leading to acute alveolitis and then to pulmonary fibrosis [25‒27]. Continuous efforts for PQ detoxification have been made for decades and a panel of patents has been granted, some of which are summarized in Table 1. These potential therapeutic candidates show protective effects on PQ poisoning at least in different animal models (acute lung injury model, pulmonary fibrosis model, liver injury model, Parkinson’s model, etc.). Although the protective effect of the candidates in these patents is promising, their translational potentials need further evaluation. Firstly, nearly all of them lack clinical evidence, and the detoxification was performed only on mice or rats. Secondly, some of them have limited clinical significance. For example, the candidate compounds were pre-treated to animals several times or days before the PQ insult. However, the clinical reality is that nobody can predict PQ poisoning and thus pre-medicate. Nor does anyone would like to take medication in advance to prevent PQ poisoning. Thus, for these patents and studies mentioned as follows, the flaws in the experimental design flaws decrease the feasibility of PQ detoxification. In addition, the safety of many candidates has not been evaluated.
| Application No. | Compounds | PQ dose | Indication | Year |
|---|---|---|---|---|
| CN114848621A | Lysine (dose not shown), co-treatment | Mice, i.p., dose not shown | Improved lung fibrosis and reduced mortality in mice | 2023 |
| CN112716923A | Octacosanol (200, 300 and 500 mg/kg), post-treatment | Mice, p.o., 100 mg/kg | Improves collagen deposition and fibrosis in the lungs of mice | 2021 |
| CN111374966A | Mildronate (100–600 mg/kg), post-treatment | Rats, p.o., 160 mg/kg | Improves pulmonary fibrosis in mice | 2020 |
| CN111228259A | 5-Hydroxy-1-methylhydantoin (100 mg/kg), pre-treatment | Mice, p.o., 25 mg/kg | Improves lung injury in mice | 2020 |
| CN110859837A | cucurbituril [7] (2.71 g/kg), co-treatment | Mice, p.o., 300 mg/kg | Increase the survival rate of PQ-intoxicated mice at supra-lethal doses, reduce PQ absorption and tissue distribution, and alleviate PQ-induced toxicity | 2020 |
| WO2021057721A1 | 6-disulfonic acid or 9,10-anthrahydroquinone-2,6-disulfonate (30–60 mmol/L, 5–10 mL), post-treatment | Rats, p.o., 200 mg/kg | Improves lung injury in mice | 2019 |
| CN109875992A | FSK (2.5, 5 mg/kg), DFSK (5, 10 mg/kg), pre-treatment | Mice, i.p., 20 mg/kg | Improves pulmonary fibrosis in mice | 2019 |
| CN107951871A | Glycosyl-modified polyphenol compounds (800 mg/kg), post-treatment | Mice, i.p., 300 mg/kg | Reduces oxidative stress levels and improves lung injury | 2018 |
| CN105748494A | Polydatin (5, 10, 20 mg/kg), post-treatment | Rats, p.o., 50 mg/kg | Improves pulmonary fibrosis in rats | 2016 |
| CN104922277A | fructus schizandrae extract (200, 400, 800 mg/kg), post-treatment | Mice, p.o., 300 mg/kg | Improves lung injury in mice | 2015 |
Data were collected from the European Patent Office database: http://ep.espacenet.com/.
3.2. Potential Leads in Publications
PQ poisoning can cause systemic damage to the body. The mechanisms of PQ-induced toxicity are extremely complex and multi-targeted. According to the literature, the main ones involved are oxidative stress, inflammation, mitochondrial damage, and apoptosis [28]. By the same mechanism, PQ can damage the intestinal tract, affect the heart and kidneys, as well as attack the nervous and immune systems, leading to multi-organ failure. Drugs and compounds that have the potential for PQ detoxification are summarized in Figure 2.
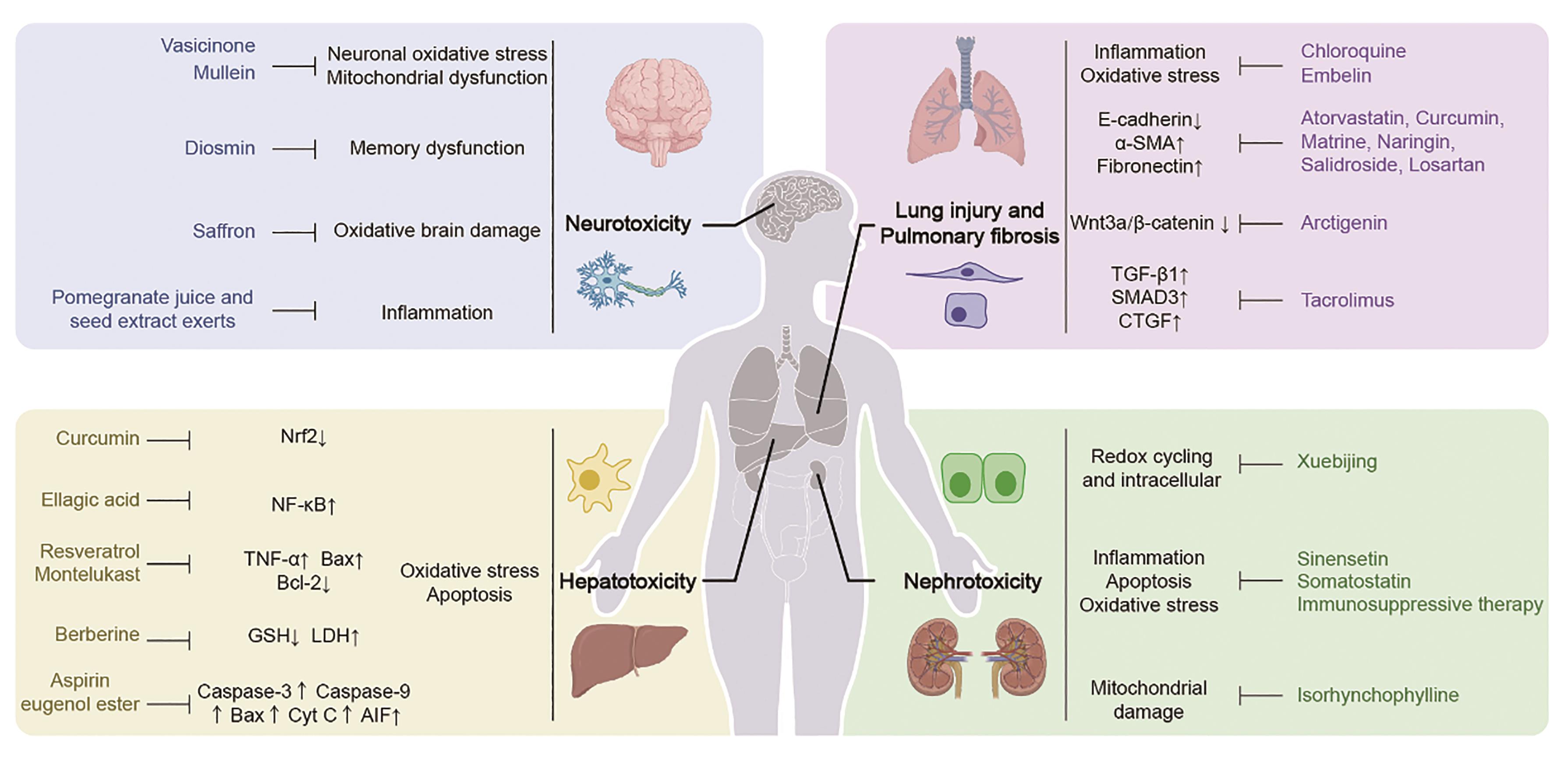
Figure 2. The potential drugs and compounds with protective effects against paraquat-induced toxicity in different organs. 995 × 471 mm (59 × 59 DPI).
3.2.1. Paraquat Lung Injury and Lung Fibrosis
PQ poisoning triggers an oxidative cycle in the lung, resulting in the continuous production of reactive oxygen species (ROS) and oxidative stress [29]. Under oxidative stress, pro-inflammatory factors are activated in lung cells. PQ toxicity mainly targets alveolar epithelial cells, damaging mitochondria and endoplasmic reticulum and causing lung damage [30,31]. ROS activates the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) signaling pathway, causing the activation of various pro-inflammatory factors and thus triggering acute alveolitis [32]. Chloroquine (CQ) is a potent lysosomal weak base for the treatment of malaria. In PQ-induced lung injury, CQ protects the lung injury by reducing inflammation and oxidative stress [33]. Embelin is a hydroxybenzoquinone with multiple pharmacological activities. Embelin inhibits PQ-induced NF-κB activation, decreases pro-inflammatory cytokines release, and protects against PQ-induced lung injury [34].
PQ-induced lung injury leads to alveolar detachment and pulmonary oedema, followed by fibroblast proliferation that fills the alveolar space, resulting in lung fibrosis [35]. Epithelial-mesenchymal transition (EMT) plays an important role in PQ-induced lung fibrosis. PQ significantly regulates the expression of EMT biomarkers E-cadherin, vimentin, and alpha-smooth muscle actin(α-SMA). PQ-induced EMT is mainly via the transforming growth factor beta (TGF-β)/small mother against decapentaplegic (SMAD) signaling pathway [36]. Many natural products (curcumin [36], matrine [37], naringin [38], salidroside [39]) and small molecule inhibitors (losartan [40], rapamycin [41]) are shown to inhibit PQ-induced pulmonary fibrosis by inhibiting TGFβ1-dependent EMT. Interestingly, a few antibiotics are found to alleviate PQ-induced pulmonary fibrosis. Doxycycline, a tetracyclic antibiotic used in the treatment of infectious diseases, inhibits PQ-induced EMT in alveolar epithelial cells by downregulating the TGF-β signaling pathway [42]. The immunosuppressive drug tacrolimus reduces PQ-induced lung injury and fibrosis by inhibiting pro-fibroinflammatory factors (TGF-β1, SMAD3, and connective tissue growth factor (CTGF)) and increasing SMAD7 expression [43]. Significant activation of Wnt signaling during PQ-induced fibrosis was observed [44] and arctigenin, a lignan isolated from certain plants of the Asteraceae, alleviates PQ-induced EMT by regulating the Wnt3a/β-catenin signaling pathway [45].
3.2.2. Paraquat Hepatotoxicity
Oxidative stress and apoptosis caused by PQ poisoning can damage liver function, and trigger liver fibrosis, inflammatory response, and liver failure [31,46]. During this process, the NF-κB is activated and translocated to the nucleus to promote the expression of pro-inflammatory cytokines [47]. Ellagic acid, a natural compound with anti-inflammatory and antioxidant effects, alleviates PQ-induced cellular oxidative stress and apoptosis and improves damaged liver function by inhibiting the NF-κB signaling [48]. In addition, PQ-induced oxidative stress can dissociate nuclear factor erythroid 2-related factor 2 (Nrf2) from kelch-like ECH-associated protein 1 (KEAP1). Curcumin, a Nrf2 inducer, inhibits PQ-induced oxidative stress in liver cells by up-regulating Nrf2 protein and protects PQ-induced liver tissue damage [49]. Glutathione (GSH) has the function of maintaining cellular redox balance and exerts antioxidant functions by consuming oxidative stress. PQ poisoning causes oxidative stress in liver cells, resulting in a decrease in GSH levels. Berberine (BBR) is a famous natural product with multiple biological activities such as anti-tumor, anti-inflammatory, and liver and kidney protective effect [49,50]. BBR exerts its antioxidant capacity by increasing the GSH activity in rat liver tissue and serum and inhibits PQ-induced liver damage [51]. Other compounds such as aspirin eugenol ester [52], nobiletin [53], and vitamins C and E [54] also show protective effects against PQ-induced liver injury.
3.2.3. Paraquat Nephrotoxicity
Accumulation of PQ in the kidneys can cause severe nephrotoxicity, leading to decreased renal function and kidney damage [55]. PQ toxicity causes vacuolization of proximal tubular cells and tubular necrosis [56]. PQ is quickly absorbed after ingestion and most of it is eliminated through the kidneys in its original form [10] which results in a high concentration of PQ in the kidney triggering cell apoptosis and oxidative stress and leading to renal dysfunction [3]. Sinensetin, a flavonoid with anti-inflammatory, anti-tumor, and antioxidant activities, alleviates the nephrotoxic effects of PQ in rats and improves renal tubular deterioration and tubular necrosis [57]. Somatostatin alleviates renal damage caused by PQ poisoning by inhibiting oxidative stress, inflammatory response, and apoptosis [58]. Isorhynchophylline (IRN) has anti-inflammatory and antioxidant activities in cardiovascular and brain diseases. IRN attenuated PQ-induced oxidative stress and mitochondrial damage through upregulation of toll-interacting protein (Tollip) and improved acute kidney injury in rats [59].
3.2.4. Paraquat Neurotoxicity
PQ is a potential neurotoxin [60]. PQ forms ROS and oxidative stress causing cell damage and neurotoxicity [61]. PQ inhibits the proliferation of mouse neural progenitor cells in a concentration-dependent manner, and reduces the differentiation of neurons and the migration distance of neurospheres, leading to neurogenesis impairment [62]. Crocin, a spice extracted from the dried stigmas of the plant crocus, has a protective effect on lipopolysaccharide-induced acute lung injury and dimethyl nitrosamine-induced liver injury in mice [63]. In PQ-induced neurotoxicity, crocin protected rats from PQ-induced oxidative brain damage through its antioxidant effect [64]. PQ exposure may lead to structural and functional impairment of midbrain neurons and increase the risk of neurodegenerative diseases, particularly Parkinson’s disease [65,66]. Epidemiological studies showed that people exposed to low-dose PQ for a long time have a 1.3–3.6 times higher risk of Parkinson’s disease than the general population [67]. Oral administration of diosmin, a flavonoid compound found in various plants, effectively improves memory dysfunction in rats caused by PQ [68]. Vasicinone induces mitophagy by activating the PINK1-Parkin signaling pathway and improves PQ-mediated neuronal cell damage [69]. Mullein plays a protective role against PQ-induced neurodegeneration by improving mitochondrial function and regulating autophagy, thereby reducing cell death and apoptosis of dopaminergic neurons [70]. The neurotoxicity of PQ may promote inflammatory responses and induce DNA fragmentation. Pomegranate (Punica granatum L.) juice and seed extract exerts its preventive effect on PQ-induced Parkinson’s disease through its antioxidant, anti-inflammatory, and anti-apoptotic effects [71].
4. Future Research Directions
The main reason for the lack of breakthroughs in the development of PQ detoxifying drugs is that we lack in-depth studies on the mechanisms of PQ toxicity. Novel techniques, such as “omics”, provide strong support for the discovery of PQ antidotes (Figure 3). In addition, from pharmacoeconomic considerations, drug repurposing is one of the practical strategies.
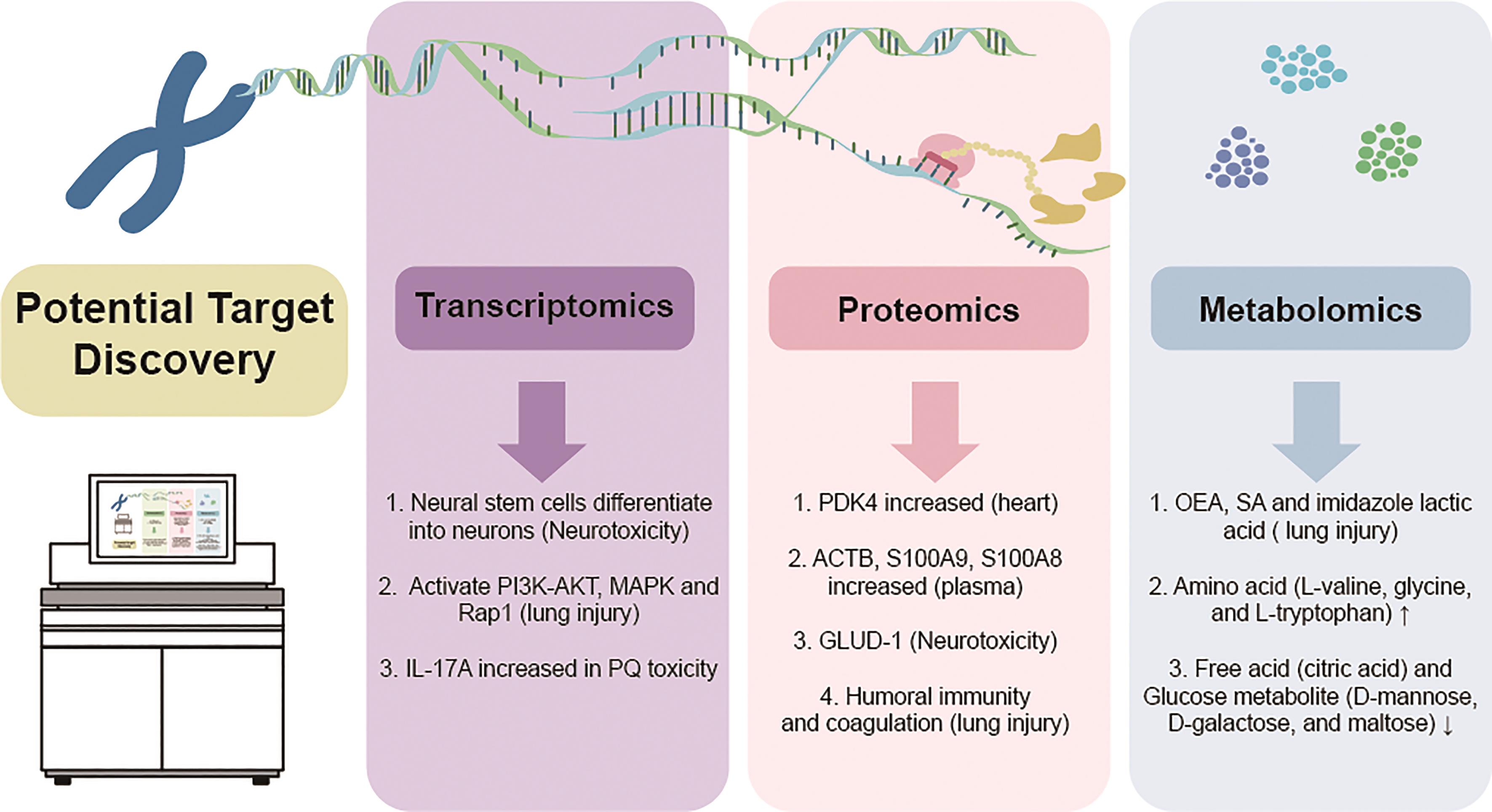
Figure 3. Methods for discovery of potential targets of paraquat toxicity. 437 × 238 mm (59 × 59 DPI).
4.1. Target Exploration
4.1.1. Transcriptomics
Transcriptomics can reflect the expression and regulation of genes in cells or tissues from a global level. It is the earliest and most widely used omics technology. Transcription levels can largely reflect the expression levels of genes and can be used to explore biomarkers and study the pathogenesis of diseases [72]. A single-cell RNA-seq (scRNA-seq) assay was performed to detect the impact of PQ toxicity on the differentiation of primary mouse neural stem cells. The results show that PQ poisoning causes mouse neural stem cells to differentiate into neurons, providing new insights into the study of antidotes for PQ’s neurotoxicity [73]. An RNA-seq sequencing assay in PQ-induced pulmonary fibrosis in rats showed that PQ poisoning was complex and mainly enriched in the phosphoinositide 3-kinases (PI3K)-AKT, mitogen-activated protein kinase (MAPK), and Rap1 signaling pathways [74]. Anthrahydroquinone-2,6-disulfonate (AH2QDS) affects the PI3K-AKT signaling pathway and cGMP-PKG signaling pathway, reducing the absorption of PQ in rats while reducing intracellular oxidative stress and slowing down acute lung injury. This information provides a theoretical basis for the development of PQ antidote [74,75]. A scRNA-seq assay reveals genetic changes in the brain tissue of PQ-induced Parkinson’s disease (PD) mice and found that the distinct molecular gene marker in glutamatergic neurons, slc17a6 may be potential therapeutic targets for PQ-induced PD depression [76]. A whole-genome sequencing on mice with PQ-induced pulmonary fibrosis found that the pro-inflammatory cytokine interleukin-17A (IL-17A) plays an important role in the mechanism of PQ poisoning. Mesenchymal stem cells (MSC) can effectively reduce IL-17A levels and reduce PQ toxicity, providing molecular fundamentals for clinical research on MSC transplantation to treat PQ poisoning [77].
4.1.2. Proteomics
Proteomics mainly studies the genes and proteins of samples and then performs data analysis and bioinformatics analysis [78]. Proteomic approaches have been used to study the mechanism of PQ poisoning and to explore the molecular target of PQ. Cardiac proteomics using quantitative tandem mass spectrometry assay showed that moderate to high doses of PQ induced the expression of pyruvate dehydrogenase kinase 4 (PDK4) in mouse hearts [77]. Untargeted and targeted proteomics was integrated to reveal differences in the expression of plasma proteins in poisoned patients. The expression of β-actin (ACTB) and small Ca2+ binding proteins (S100A9 (Myeloid-related Protein (MRP)14) and S100A8 (MRP8)) were significantly increased in the plasma of PQ poisoning patients. ACTB may be a potential target of PQ poisoning providing a new research direction for further exploring the mechanism of PQ toxicity [79]. A tandem mass spectrometry tag technology (TMT) to detect protein expression in PQ-induced lung injury found that PQ-induced lung injury was mainly related to humoral immunity and coagulation [80]. A quantitative proteomic analysis found that PQ-induced apoptosis in PC-12 cells leads to the upregulation of antioxidant function (peroxiredoxin-4 (Prdx-4), and glutamate dehydrogenase 1 (Glud-1). Customized peptides using snake venom neurotrophin molecules effectively reduce the production of intracellular ROS, and inhibit oxidative stress and apoptosis caused by PQ poisoning [81].
4.1.3. Metabolomics
Metabolomics, a technology developed after transcriptomics and proteomics that focuses on small molecule metabolites, has been widely used in genetic analysis of disease metabolic disorders, clinical biomarker screening, discovery of new treatment targets, and disease diagnosis [82]. Metabolic changes in lung injury caused by PQ poisoning in rats showed that oleoylethanolamine (OEA), stearic acid (SA), and imidazole lactate were potential biomarkers of PQ-induced lung injury [83]. Increased levels of amino acid (L-valine, glycine, and L-tryptophan) and decreased levels of free acid (citric acid) and glucose metabolite (D-mannose, D-galactose, and maltose) were observed in the PQ poisoning rat model of fibrosis. Xuebijing (XBJ) injection could significantly reverse the alterations of these three types of metabolites and fibrosis [84]. A metabolomic analysis of the serum of mice poisoned with PQ showed that the level of isopropyl alcohol (IPA) in serum was reduced in acutely PQ poisoned mice. It is speculated that the reduction of antioxidant serum metabolites caused by PQ poisoning may be a new mechanism of PQ toxicity, providing a new biomarker for the diagnosis of PQ poisoning [85]. Strengthening metabolomic research on PQ toxicity will help analyze the synthesis and transport of key metabolites, provide clues for the clinical diagnosis and treatment of PQ poisoning search for biomarkers and drug targets, improve treatment efficiency, and achieve precision medicine [86].
4.2. Drug Repurposing
Drug repurposing, a process of identifying new indications for existing drugs, is an effective strategy for drug discovery. The detoxification of PQ through drug repurposing has been reported recently. For example, atorvastatin, a widely used lipid-lowering agent, alleviates PQ-induced EMT by downregulating HIF-1α [87]. Montelukast, a medication used to control asthma, reduces PQ-induced oxidative stress and apoptosis and liver damage when treated with resveratrol [31]. A total of 33 clinical agents with therapeutic potential to detoxify PQ have been systematically reviewed recently [88]. Therefore, drug repurposing may represent a promising direction for exploring the PQ detoxification agents.
5. Conclusion
In summary, PQ is a very good herbicide, which has made an important contribution to the development of world agriculture. However, it is unfortunate that its use has been banned due to its toxicity (although PQ is not very toxic from a toxicological point of view). For decades, there has been no breakthrough in the development of PQ antidotes thus making the existence of PQ antidotes skeptical. We believe that the real difficulty in the development of PQ antidotes lies in the fact that the molecular target of PQ has not yet been clearly defined. Besides, a detailed dissection of the ADME/T processes of PQ in humans adds another layer of chances of success. Transporters and enzymes based strategies against PQ toxicity have already been proposed [89]. The philosophical concept of Chinese medicine believes that everything in the world is mutual generation and neutralize each other. Aided by novel technologies, the confirmation of the molecular targets of PQ toxicity will eventually lead to the discovery of effective PQ detoxification drugs. Detoxification of PQ is not scooping up the moon from the water.
Author Contributions: Y.Z.: Conceptualization, Methodology, Writing—original draft. X.C.: Conceptualization, Supervision, Writing—Reviewing and Editing. All authors have read and agreed to the published version of the manuscript.
Funding: This research was supported by the Science and Technology Development Fund of Macau Special Administrative Region (0081/2021/A2).
Institutional Review Board Statement: Not applicable.
Informed Consent Statement: Not applicable.
Data Availability Statement: Not applicable.
Acknowledgments: We thank Xumei Wang (Institute of Chinese Medical Sciences, University of Macau) for helping to draft the figures.
Conflicts of Interest: The authors declare no actual or potential conflicts of interest.
Abbreviations: paraquat: PQ; chloroquine, CQ; nuclear factor kappa-light-chain-enhancer of activated B cells, NF-κB; epithelial-mesenchymal transition: EMT; alpha-smooth muscle actin, α-SMA; transforming growth factor beta, TGF-β; small mother against decapentaplegic, SMAD; connective tissue growth factor, CTGF; hypoxia-inducible factor 1 subunit alpha, toll-interacting protein, Tollip; HIF-1α; wingless-related integration site, Wnt; nuclear factor erythroid 2-related factor 2, Nrf2; kelch-like ECH-associated protein 1, KEAP1; glutathione, GSH; berberine, BBR; reactive oxygen species, ROS; single-cell RNA-seq, scRNA-seq; mitogen-activated protein kinase, MAPK; anthrahydroquinone-2,6-disulfonate, AH2QDS; Parkinson’s disease, PD; interleukin-17A, IL-17A; mesenchymal stem cells, MSC; pyruvate dehydrogenase kinase 4, PDK4; β-actin, ACTB; myeloid-related protein, MRP; tandem mass spectrometry tag technology, TMT; peroxiredoxin-4, Prdx-4; glutamate dehydrogenase 1, Glud-1; oleoylethanolamine, OEA; stearic acid, SA; isopropyl alcohol, IPA.

References
- Santos, M.S.; Schaule, G.; Alves, A.; et al. Adsorption of paraquat herbicide on deposits from drinking water networks. Chem. Eng. J. 2013, 229, 324–333. doi: 10.1016/j.cej.2013.06.008
- Abreu, J.G.; Ketpura, N.I.; Reversade, B.; et al. Connective-tissue growth factor (CTGF) modulates cell signalling by BMP and TGF-β. Nat. Cell Biol. 2002, 4, 599–604. doi: 10.1038/ncb826
- Dinis-Oliveira, R.; Duarte, J.; Sánchez-Navarro, A.; et al. Paraquat poisonings: Mechanisms of lung toxicity, clinical features, and treatment. Crit. Rev. Toxicol. 2008, 38, 13–71. doi: 10.1080/10408440701669959
- Adam, A.; Smith, L.L.; Cohen, G.M. An assessment of the role of redox cycling in mediating the toxicity of paraquat and nitrofurantoin. Environ. Health Perspect. 1990, 85, 113–117. doi: 10.1289/ehp.85-1568326
- Castello, P.R.; Drechsel, D.A.; Patel, M. Mitochondria are a major source of paraquat-induced reactive oxygen species production in the brain. J. Biol. Chem. 2007, 282, 14186–14193. doi: 10.1074/jbc.M700827200
- Koo J.-R.; Kim J.-C.; Yoon J.-W.; et al. Failure of continuous venovenous hemofiltration to prevent death in paraquat poisoning. Am. J. Kidney Dis. 2002, 39, 55–59. doi: 10.1053/ajkd.2002.29880
- Krieger, R. Hayes’ Handbook of Pesticide Toxicology; Academic Press: Cambridge, MA, USA, 2010.
- Garnier, R.; Bazire, A.; Chataigner, D. Risks of occupational paraquat exposure. A review. Arch. Occup. Dis. Occup. Med. 2003, 64, 310–324.
- Bromilow, R.H. Paraquat and sustainable agriculture. Pest Manag. Sci. Formerly Pestic. Sci. 2004, 60, 340–349. doi: 10.1002/ps.823
- Gawarammana, I.B.; Buckley, N.A. Medical management of paraquat ingestion. Br. J. Clin. Pharmacol. 2011, 72, 745–757. doi: 10.1111/j.1365-2125.2011.04026.x
- Scherrmann, J.; Houze, P.; Bismuth, C.; et al. Prognostic value of plasma and urine paraquat concentration. Human Toxicol. 1987, 6, 91–93. doi: 10.1177/096032718700600116
- Roberts, D.M.; Wilks, M.F.; Roberts, M.S.; et al. Changes in the concentrations of creatinine, cystatin C and NGAL in patients with acute paraquat self-poisoning. Toxicol. Lett. 2011, 202, 69–74. doi: 10.1016/j.toxlet.2011.01.024
- Hong S.-Y.; Yang J.-O.; Lee E.-Y.; et al. Effect of haemoperfusion on plasma paraquat concentration in vitro and in vivo. Toxicol. Ind. Health 2003, 19, 17–23. doi: 10.1191/0748233703th171oa
- Lin J.-L.; Leu M.-L.; Liu Y.-C.; et al. A prospective clinical trial of pulse therapy with glucocorticoid and cyclophosphamide in moderate to severe paraquat-poisoned patients. Am. J. Respir. Crit. Care Med. 1999, 159, 357–360. doi: 10.1164/ajrccm.159.2.9803089
- Li, C.; Hu, D.; Xue, W.; et al. Treatment outcome of combined continuous venovenous hemofiltration and hemoperfusion in acute paraquat poisoning: A prospective controlled trial. Crit. Care Med. 2018, 46, 100–107. doi: 10.1097/CCM.0000000000002826
- Edith, C.; Pond, H.; Pond, S. Failure of hemoperfusion and hemodialysis to prevent death in paraquat poisoning: A retrospective review of 45 patients. Med. Toxicol. 1988, 3, 64–71. doi: 10.1007/BF03259932
- Shi, M.; Zeng, M.; Jian, T.; et al. A mass event of paraquat poisoning via inhalation. Front. Public Health 2023, 11, 1309708. doi: 10.3389/fpubh.2023.1309708
- Han Y.-Y.; Sun W.-Z. An evidence-based review on the use of corticosteroids in peri-operative and critical care. Acta Anaesthesiol. Sin. 2002, 40, 71–80.
- Xu Y.-G.; Lu Y.-Q. Systematic review and meta-analysis of the efficacy and safety of immunosuppressive pulse therapy in the treatment of paraquat poisoning. J. Zhejiang Uni.-Sci. B 2019, 20, 588–597. doi: 10.1631/jzus.B1800640
- Chen G.-H.; Lin J.-L.; Huang Y.-K. Combined methylprednisolone and dexamethasone therapy for paraquat poisoning. Crit. Care Med. 2002, 30, 2584–2587. doi: 10.1097/00003246-200211000-00030
- Kwon, W.Y.; Jo, Y.H.; Song, H.G.; et al. Antioxidant Therapy of the Paraquat Intoxication. J. Korean Soc. Emerg. Med. 2001, 12, 475–479.
- Hu, S.; Qiao, C.; Yuan, Z.; et al. Therapy with high‑dose long‑term antioxidant free radicals for severe paraquat poisoning: A pilot study. Exp. Ther. Med. 2018, 16, 5149–5155. doi: 10.3892/etm.2018.6823
- Hong S.-Y.; Hwang K.-Y.; Lee E.-Y.; et al. Effect of vitamin C on plasma total antioxidant status in patients with paraquat intoxication. Toxicol. Lett. 2002, 126, 51–59. doi: 10.1016/S0378-4274(01)00431-3
- Hong, S.Y.; Yang, J.O.; Lee, E.Y.; et al. Effects of N-acetyl-L-cysteine and glutathione on antioxidant status of human serum and 3T3 fibroblasts. J. Korean Med. Sci. 2003, 18, 649–654. doi: 10.3346/jkms.2003.18.5.649
- Dinis-Oliveira, R.; Sousa, C.; Remiao, F.; et al. Full survival of paraquat-exposed rats after treatment with sodium salicylate. Free Radical Biol. Med. 2007, 42, 1017–1028. doi: 10.1016/j.freeradbiomed.2006.12.031
- Dearden, L.C.; Fairshter, R.; McRae, D.; et al. Pulmonary ultrastructure of the late aspects of human paraquat poisoning. Am. J. Pathol. 1978, 93, 667.
- Dearden, L.C.; Fairshter, R.D.; Morrison, J.T.; et al. Ultrastructural evidence of pulmonary capillary endothelial damage from paraquat. Toxicology 1982, 24, 211–222. doi: 10.1016/0300-483X(82)90003-8
- Chen, Q.; Zhang, X.; Zhao, J.Y.; et al. Oxidative damage of the male reproductive system induced by paraquat. J. Biochem. Mol. Toxicol. 2017, 31, e21870. doi: 10.1002/jbt.21870
- Blanco-Ayala, T.; Andérica-Romero, A.; Pedraza-Chaverri, J. New insights into antioxidant strategies against paraquat toxicity. Free Radical Res. 2014, 48, 623–640. doi: 10.3109/10715762.2014.899694
- Dilberger, B.; Baumanns, S.; Schmitt, F.; et al. Mitochondrial oxidative stress impairs energy metabolism and reduces stress resistance and longevity of C. elegans. Oxid. Med. Cell. Longevity 2019, 2019, 6840540. doi: 10.1155/2019/6840540
- El-Boghdady, N.A.; Abdeltawab, N.F.; Nooh, M.M. Resveratrol and montelukast alleviate paraquat-induced hepatic injury in mice: Modulation of oxidative stress, inflammation, and apoptosis. Oxid. Med. Cell. Longevity 2017, 2017, 9396425. doi: 10.1155/2017/9396425
- Wang, X.; Luo, F.; Zhao, H. Paraquat-induced reactive oxygen species inhibit neutrophil apoptosis via a p38 MAPK/NF-κB–IL-6/TNF-α positive-feedback circuit. PLoS ONE 2014, 9, e93837. doi: 10.1371/journal.pone.0093837
- Shen, H.; Wu, N.; Wang, Y.; et al. Chloroquine attenuates paraquat-induced lung injury in mice by altering inflammation, oxidative stress and fibrosis. Int. Immunopharmacol. 2017, 46, 16–22. doi: 10.1016/j.intimp.2017.02.020
- SreeHarsha, N. Embelin impact on paraquat‐induced lung injury through suppressing oxidative stress, inflammatory cascade, and MAPK/NF‐κB signaling pathway. J. Biochem. Mol. Toxicol. 2020, 34, e22456. doi: 10.1002/jbt.22456
- Subbiah, R.; Tiwari, R.R. The herbicide paraquat-induced molecular mechanisms in the development of acute lung injury and lung fibrosis. Crit. Rev. Toxicol. 2021, 51, 36–64. doi: 10.1080/10408444.2020.1864721
- Tyagi, N.; Singh, D.; Dash, D.; et al. Curcumin modulates Paraquat-induced epithelial to Mesenchymal transition by regulating transforming growth factor-β (TGF-β) in A549 cells. Inflammation 2019, 42, 1441–1455. doi: 10.1007/s10753-019-01006-0
- Li M.-Q.; Deng, J.; Wang S.-P. Matrine alleviates paraquat-induced pulmonary fibrosis in mouse models. Basic Clin. Med. 2022, 42, 1385.
- Chen, Y.; Nie Y.-C.; Luo Y.-L.; et al. Protective effects of naringin against paraquat-induced acute lung injury and pulmonary fibrosis in mice. Food Chem. Toxicol. 2013, 58, 133–140. doi: 10.1016/j.fct.2013.04.024
- Zhang, Z.; Ding, L.; Wu, L.; et al. Salidroside alleviates paraquat-induced rat acute lung injury by repressing TGF-β1 expression. Int. J. Clin. Exp. Path. 2014, 7, 8841.
- Guo, F.; Sun, Y.; Su, L.; et al. Losartan attenuates paraquat-induced pulmonary fibrosis in rats. Hum. Exp. Toxicol. 2015, 34, 497–505. doi: 10.1177/0960327114543840
- Shao, X.; Li, M.; Luo, C.; et al. Effects of rapamycin against paraquat-induced pulmonary fibrosis in mice. J. Zhejiang Univ.-Sci. B 2015, 16, 52–61. doi: 10.1631/jzus.B1400229
- Hua X.-F.; Li X.-H.; Li M.-M.; et al. Doxycycline attenuates paraquat-induced pulmonary fibrosis by downregulating the TGF-β signaling pathway. J. Thorac. Dis. 2017, 9, 4376. doi: 10.21037/jtd.2017.10.42
- Ren, Y.; Jian, X.; Zhang, Z.; et al. Effects of tacrolimus on the TGF‑β1/SMAD signaling pathway in paraquat‑exposed rat alveolar type II epithelial cells. Mol. Med. Rep. 2020, 22, 3687–3694. doi: 10.3892/mmr.2020.11453
- Yang, Z.; Wang, M.; Ren, Y.; et al. Inhibition of Wnt10b/β-catenin signaling alleviates pulmonary fibrogenesis induced by paraquat in vivo and in vitro. Life Sci. 2021, 286, 120027. doi: 10.1016/j.lfs.2021.120027
- Gao, F.; Zhang, Y.; Yang, Z.; et al. Arctigenin suppressed epithelial-mesenchymal transition through Wnt3a/β-catenin pathway in PQ-induced pulmonary fibrosis. Front. Pharmacol. 2020, 11, 584098. doi: 10.3389/fphar.2020.584098
- Liu, H.; Wu, Q.; Chu, T.; et al. High-dose acute exposure of paraquat induces injuries of swim bladder, gastrointestinal tract and liver via neutrophil-mediated ROS in zebrafish and their relevance for human health risk assessment. Chemosphere 2018, 205, 662–673. doi: 10.1016/j.chemosphere.2018.04.151
- Hoffmann, A.; Baltimore, D. Circuitry of nuclear factor κB signaling. Immunol. Rev. 2006, 210, 171–186. doi: 10.1111/j.0105-2896.2006.00375.x
- Qi, M.; Wang, N.; Xiao, Y.; et al. Ellagic acid ameliorates paraquat-induced liver injury associated with improved gut microbial profile. Environ. Pollut. 2022, 293, 118572. doi: 10.1016/j.envpol.2021.118572
- Kheiripour, N.; Plarak, A.; Heshmati, A.; et al. Evaluation of the hepatoprotective effects of curcumin and nanocurcumin against paraquat‐induced liver injury in rats: Modulation of oxidative stress and Nrf2 pathway. J. Biochem. Mol. Toxicol. 2021, 35, e22739. doi: 10.1002/jbt.22739
- Othman, M.S.; Safwat, G.; Aboulkhair, M.; et al. The potential effect of berberine in mercury-induced hepatorenal toxicity in albino rats. Food Chem. Toxicol. 2014, 69, 175–181. doi: 10.1016/j.fct.2014.04.012
- Eftekhari, A.; Hasanzadeh, A.; Khalilov, R.; et al. Hepatoprotective role of berberine against paraquat-induced liver toxicity in rat. Environ. Sci. Pollut. Res. Int. 2020, 27, 4969–4975. doi: 10.1007/s11356-019-07232-1
- Zhang Z.-D.; Yang Y.-J.; Liu X.-W.; et al. The protective effect of aspirin eugenol ester on paraquat-induced acute liver injury rats. Front. Med. 2020, 7, 589011. doi: 10.3389/fmed.2020.589011
- Ijaz, M.U.; Batool, M.; Ashraf, A.; et al. A study on the curative effect of nobiletin on paraquat induced toxicity in rat. J. King Saud Univ.-Sci. 2022, 34, 101673. doi: 10.1016/j.jksus.2021.101673
- Okolonkwo, B.N. The Role of Vitamin E in Hepatophysiology of Paraquat Induced Toxicity. Res. J. Gastroenterol. Hepatol. 2022, 5, 119–125.
- Kim S.-J.; Gil H.-W.; Yang J.-O.; et al. The clinical features of acute kidney injury in patients with acute paraquat intoxication. Nephrol. Dial. Transplant. 2009, 24, 1226–1232. doi: 10.1093/ndt/gfn615
- Xu, J.; Zhen, J.; Tang, L.; et al. Intravenous injection of Xuebijing attenuates acute kidney injury in rats with paraquat intoxication. World J. Emerg. Med. 2017, 8, 61. doi: 10.5847/wjem.j.1920-8642.2017.01.011
- Ijaz, M.U.; Manzoor, A.; Hamza, A.; et al. Ameliorative potential of sinensetin against paraquat induced renal damage by regulating oxidative, inflammatory, apoptotic and histopathological profile in male albino rats. Eur. J. Inflamm. 2024, 22, 1–9. doi: 10.1177/1721727X241233122
- Yang, Z.; Cao, K.; Xu, C.; et al. Study on the protective effect and mechanism of somatostatin on renal injury in paraquat intoxicated mice. Chin. J. Ind. Hyg. Occup. Dis. 2020, 38, 410–415.
- Zheng, Q.; Zhang, Y.; Zhao, Z.; et al. Isorhynchophylline ameliorates paraquat-induced acute kidney injury by attenuating oxidative stress and mitochondrial damage via regulating toll-interacting expression. Toxicol. Appl. Pharmacol. 2021, 420, 115521. doi: 10.1016/j.taap.2021.115521
- McCormack, A.L.; Atienza, J.G.; Johnston, L.C.; et al. Role of oxidative stress in paraquat‐induced dopaminergic cell degeneration. J. Neurochem. 2005, 93, 1030–1037. doi: 10.1111/j.1471-4159.2005.03088.x
- Bus, J.S.; Gibson, J.E. Paraquat: Model for oxidant-initiated toxicity. Environ. Health Perspect. 1984, 55, 37–46. doi: 10.1289/ehp.845537
- Zhang, B.; Zhang, Y.; Zuo, Z.; et al. Paraquat-induced neurogenesis abnormalities via Drp1-mediated mitochondrial fission. Ecotoxicol. Environ. Saf. 2023, 257, 114939. doi: 10.1016/j.ecoenv.2023.114939
- Yang, R.; Yang, L.; Shen, X.; et al. Suppression of NF-κB pathway by crocetin contributes to attenuation of lipopolysaccharide-induced acute lung injury in mice. Eur. J. Pharmacol. 2012, 674, 391–396. doi: 10.1016/j.ejphar.2011.08.029
- Daneshvar, A.; Jouzdani, A.F.; Firozian, F.; et al. Neuroprotective effects of crocin and crocin-loaded niosomes against the paraquat-induced oxidative brain damage in rats. Open Life Sci. 2022, 17, 1174–1181. doi: 10.1515/biol-2022-0468
- Suk, W.A.; Ahanchian, H.; Asante, K.A.; et al. Environmental pollution: An under-recognized threat to children’s health, especially in low-and middle-income countries. Environ. Health Perspect. 2016, 124, A41–A45. doi: 10.1289/ehp.1510517
- Berry, C.; La Vecchia, C.; Nicotera, P. Paraquat and Parkinson’s disease. Cell Death Differ. 2010, 17, 1115–1125. doi: 10.1038/cdd.2009.217
- Vaccari, C.; El Dib, R.; Gomaa, H.; et al. Paraquat and Parkinson’s disease: A systematic review and meta-analysis of observational studies. J. Toxicol. Environ. Health Part B 2019, 22, 172–202. doi: 10.1080/10937404.2019.1659197
- Mirshekar, M.A.; Miri, S.; Shahraki, A. A survey of the effects of diosmin on learning and memory following the use of paraquat herbicide poisoning in a model of rats. Shiraz E-Med. J. 2020, 21, e94143. doi: 10.5812/semj.94143
- Huang C.-Y.; Sivalingam, K.; Shibu, M.A.; et al. Induction of autophagy by vasicinone protects neural cells from mitochondrial dysfunction and attenuates paraquat-mediated Parkinson’s disease associated α-synuclein levels. Nutrients 2020, 12, 1707. doi: 10.3390/nu12061707
- Chaouhan, H.S.; Li, X.; Sun K.-T.; et al. Calycosin alleviates paraquat-induced neurodegeneration by improving mitochondrial functions and regulating autophagy in a drosophila model of Parkinson’s disease. Antioxidants 2022, 11, 222. doi: 10.3390/antiox11020222
- Fathy, S.M.; El-Dash, H.A.; Said, N.I. Neuroprotective effects of pomegranate (Punica granatum L.) juice and seed extract in paraquat-induced mouse model of Parkinson’s disease. BMC Complement. Med. Ther. 2021, 21, 130. doi: 10.1186/s12906-021-03298-y
- Hrdlickova, R.; Toloue, M.; Tian, B. RNA‐Seq methods for transcriptome analysis. Wiley Interdiscip. Rev. RNA 2017, 8, e1364. doi: 10.1002/wrna.1364
- Xiong, G.; Zhang, B.; Song, B.; et al. Single-cell RNA sequencing reveals adverse effects of paraquat on the fate commitment of murine neural stem cells. Sci. Total Environ. 2021, 785, 147386. doi: 10.1016/j.scitotenv.2021.147386
- Li, N.; Huang, Y.; Yi, Y.; et al. Analysis of abnormal expression of signaling pathways in PQ-induced acute lung injury in SD rats based on RNA-seq technology. Inhalation Toxicol. 2024, 36, 1–12. doi: 10.1080/08958378.2023.2300373
- Qian, J.; Wu C.-Y.; Wu D.-M.; et al. Anthrahydroquinone-2-6-disulfonate is a novel, powerful antidote for paraquat poisoning. Sci. Rep. 2021, 11, 20159. doi: 10.1038/s41598-021-99591-4
- Weng, Y.; Zhang, Y.; Li, Y.; et al. Single-cell RNA-sequencing of cellular heterogeneity and pathogenic mechanisms in paraquat-induced Parkinson’s disease with depression. Ecotox. Environ. Safe. 2024, 273, 116169. doi: 10.1016/j.ecoenv.2024.116169
- Zhang, L.; Wang, Y.; Shen, H.; et al. Combined signaling of NF-kappaB and IL-17 contributes to Mesenchymal stem cells-mediated protection for Paraquat-induced acute lung injury. BMC Pulm. Med. 2020, 20, 1–10. doi: 10.1186/s12890-020-01232-5
- Aslam, B.; Basit, M.; Nisar, M.A.; et al. Proteomics: Technologies and their applications. J. Chromatogr. Sci. 2017, 55, 182–196. doi: 10.1093/chromsci/bmw167
- Zhang, T.; Huang, S.; Wang, M.; et al. Integrated untargeted and targeted proteomics to unveil plasma prognostic markers for patients with acute paraquat poisoning: A pilot study. Food Chem. Toxicol. 2023, 182, 114187. doi: 10.1016/j.fct.2023.114187
- Peng, J.; Liu, Z.; Zhou, Y.; et al. Proteomic analysis of lung injuries induced by paraquat in mice. Chin. J. Emerg. Med. 2021, 12, 1318–1323.
- Madhubala, D.; Patra, A.; Islam, T.; et al. Snake venom nerve growth factor-inspired designing of novel peptide therapeutics for the prevention of paraquat-induced apoptosis, neurodegeneration, and alteration of metabolic pathway genes in the rat pheochromocytoma PC-12 cell. Free Radical Biol. Med. 2023, 197, 23–45. doi: 10.1016/j.freeradbiomed.2023.01.019
- Fiehn, O. Metabolomics by gas chromatography–mass spectrometry: Combined targeted and untargeted profiling. Curr. Protoc. Mol. Biol. 2016, 114, 30–34. doi: 10.1002/0471142727.mb3004s114
- Liu, X.; Li, C.; Hou, C.; et al. Dissecting the effects of paraquat-induced pulmonary injury in rats using UPLC-Q-TOF-MS/MS-based metabonomics. Toxicol. Res. 2023, 12, 527–538. doi: 10.1093/toxres/tfad040
- Wang, T.; Li, S.; Wu, Y.; et al. Mechanistic investigation of Xuebijing for treatment of paraquat-induced pulmonary fibrosis by metabolomics and network pharmacology. ACS Omega 2021, 6, 19717–19730. doi: 10.1021/acsomega.1c02370
- Yu, Y.; Gao, Z.; Lou, J.; et al. Identification of serum-based metabolic feature and characteristic metabolites in paraquat intoxicated mouse models. Front. Physiol. 2020, 11, 65. doi: 10.3389/fphys.2020.00065
- Wen, C.; Wang, Z.; Zhang, M.; et al. Metabolic changes in rat urine after acute paraquat poisoning and discriminated by support vector machine. Biomed. Chromatogr. 2016, 30, 75–80. doi: 10.1002/bmc.3627
- Du, J.; Zhu, Y.; Meng, X.; et al. Atorvastatin attenuates paraquat poisoning-induced epithelial-mesenchymal transition via downregulating hypoxia-inducible factor-1 alpha. Life Sci. 2018, 213, 126–133. doi: 10.1016/j.lfs.2018.10.026
- Liu, X.; Yang, H.; Liu, Z. Signaling pathways involved in paraquat-induced pulmonary toxicity: Molecular mechanisms and potential therapeutic drugs. Int. Immunopharmacol. 2022, 113, 109301. doi: 10.1016/j.intimp.2022.109301
- Wang, X.; Wang, X.; Zhu, Y.; et al. ADME/T-based strategies for paraquat detoxification: Transporters and enzymes. Environ. Pollut. 2021, 291, 118137. doi: 10.1016/j.envpol.2021.118137







